Depression had been part of my life for many years, but I believed I had learned to manage it well.
I was not alone. I knew that a fifth of adults in the UK experience depression and anxiety at some time. Indeed, many of my colleagues experienced those feelings, even if not expressed in those exact words.
However, I found myself ill-prepared for the experience when I became a client of the mental health services. I had been getting medication from my doctor for depression but it didn’t seem to be working very well and my mood was getting lower, so they referred me to the community psychiatric team.
I thought no more about it but noticed how much harder it was to be doing things, both at home and work, and to deal with my responsibilities.
Being in frontline social work meant that I had to keep my wits about me and not get distracted, but the feelings of depression made this difficult. The depressive thoughts would be intrusive and distracting.
‘It was harder to make decisions’
Alongside depression came anxiety; it was harder to make decisions, so I was pleased that many casework decisions were ones I could share with my manager or colleagues. Nonetheless, this was a period when I was plagued with much self-doubt about my skills and abilities and I needed more support than normal.
It was hard to keep things in perspective and remember everything, so I became dependant on my mobile phone in order to help me keep lists of things to do and deadlines. I became over focussed on my work and getting things done, adding to my stress levels but was ever fearful that someone would find out I was feeling depressed and it would be seen as a failing.
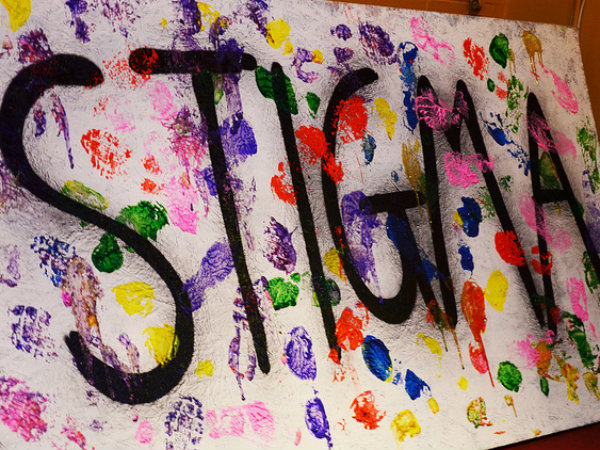
The social work profession still seems to stigmatise mental health problems in its staff, despite all the talk of offering support. I did not want to go off sick and so it was a difficult balancing act trying to keep going. At times it seemed overwhelming.
Using services
After three months I got an appointment with the mental health services and saw a community psychiatric nurse who did an initial assessment and referred me to a psychiatrist.
The psychiatrist picked up on my low mood and assessed it well, I thought. We talked about new medication and he recommended one which would be monitored by regular visits by community psychiatric nurses (CPNs).
Suddenly, I found myself in the dependent role of client, having to see the CPNs on a regular basis.
I had to juggle my working week to fit around their appointment times, which was made all the more difficult as they could only tell me the day of the visit but not the time, only a vague indication of morning or afternoon. So I had to be home for blocks of time to make sure I was in; I did much home working and had to juggle visits to clients, so often worked late to catch up.
Medication
I also became an expert on the side-effects of the new antidepressants that I was taking, and found it easy to slip into thinking that every twinge, ache or pain was due to the new drug. I longed for this phase to end, for it took some time before the drugs became effective. Those were long weeks indeed.
Depression affected my family life, too, for while my wife was very understanding, it was difficult to explain my low moods to our young children and to say the CPN was someone who came to make me feel better. They understood illness as being like a cold, which you recovered from, so I explained it in terms of “feeling sad”.
It was hard to relax and play with them, but that was something I had to force myself to do. I was able to afford private counselling and had supportive friends, which helped as I found that the focus of the CPNs was mainly about how I was responding to the medication.
It felt like they had a tick box of things that had to be covered in each visit and since it wasn’t the same person who visited each time, it was hard to form a lasting relationship. After six weeks the visits ended and after that I had to go back to my doctor for medication. It seemed that I had had my ration of service.
The hardest part
Having been a client of the mental health services helped me understand the experiences of my clients who suffer depression and anxiety and who couldn’t afford private therapy.
The hardest part was avoiding identifying with them, but rather to keep the focus on the care of their children. Part of me longed to say I was aware of their suffering but rather found myself like the CPNs were with me: professional and objective.
Even so, the human being in me wanted to reach out and help relieve their suffering so they and their family would benefit. I had to remember while the similarities helped me to understand them, it was the differences that made me able to help.
One client had waited a long time to be assessed by the mental health services and queried how desperate you had to be to get a service. I could have helped them answer that but it was best just to empathise. I told them that I’d try to get their case prioritised knowing that I could not make it happen, but hoped my gesture was of some help.
Being a client of the mental health service was a curious experience. Being dependant on a service was hard to adjust to. It showed me that we all have our vulnerable side and sometimes need extra help, like our clients, and that line can be easily crossed. None of us are fireproof.


 Bournemouth, Christchurch and Poole
Bournemouth, Christchurch and Poole  Hampshire County Council
Hampshire County Council  Lincolnshire County Council
Lincolnshire County Council  Norfolk County Council
Norfolk County Council  Northamptonshire Children’s Trust
Northamptonshire Children’s Trust  South Gloucestershire Council
South Gloucestershire Council  Wiltshire Council
Wiltshire Council  Wokingham Borough Council
Wokingham Borough Council  Children and young people with SEND are ‘valued and prioritised’ in Wiltshire, find inspectors
Children and young people with SEND are ‘valued and prioritised’ in Wiltshire, find inspectors  How specialist refugee teams benefit young people and social workers
How specialist refugee teams benefit young people and social workers  Podcast: returning to social work after becoming a first-time parent
Podcast: returning to social work after becoming a first-time parent  Podcast: would you work for an inadequate-rated service?
Podcast: would you work for an inadequate-rated service?  Family help: one local authority’s experience of the model
Family help: one local authority’s experience of the model  Workforce Insights – showcasing a selection of the sector’s top recruiters
Workforce Insights – showcasing a selection of the sector’s top recruiters 

 Facebook
Facebook X
X LinkedIn
LinkedIn Instagram
Instagram
The same sort of feeling but I learnt how to be bulletproof and officeproof
I wish you could teach me how to do that!
Thank you for sharing your experiences. A good reminder that we are all part of the communities we support.
A very honest and open account of being on the receiving end of services. We can certainly see where mental health services fail our clients time and time again due to underfunding from Government.
Thank you for opening up about your situation. I think any time we have a mental health crisis, we should always be focused on recovery. The fact that you can speak about it and sought help about it was braver than you realise. Peter Beresford, a professor of social work writes about what it is like to be a social worker who also receives support from mental health services, and is always worth a read.
Only understand being part of the community if experienced the same loss service users feel when through no fault of their own their lives are destroyed by ‘professionals’ . I am sure the profession is full of double standards
I`m sorry to hear you had such an unhelpful experience with the CPNs. I spent most of my working life in Community Mental Health Teams (I`m an AMHP, was an ASW); everyone, CPNs included, tried their best to negotiate a convenient time for home visits, particularly if the person being visited was working.
Yes, having been a young carer, then a children’s social worker, then an ASW and AMHP, I’ve been a service user too.
One of the things I have sometimes found difficult, if I’m open with mental health service colleagues about my experience of familial (paranoid schizophrenia) or personal mental health difficulties (intermittent anxiety and depression, since pre-teenage years), is the “funny look”. I don’t know whether they expect me to act out in front of them, or whether they mark me with a mental “not to be trusted” flag, but I have learnt not to tell mental health colleagues – which I think is rather sad.
I know my triggers; I understand their roots in early childhood experiences; I think they are what help to make me a sensitive and reflective,”good enough” social worker, and I recognise that they are also the source of my vulnerability as a practitioner.
Just as an addendum: I think it’s a great pity that we don’t pay more attention, as social workers and practitioners in the helping professions, to the concept of the wounded healer. It might help us all to work better for both service users and ourselves.
I like the notion of the wounded healer. I have a mental health diagnosis and am a social worker, I wouldn’t share my personal experience with every client but it has been relevant on a number of occasions and I view it as part of my toolkit as a practitioner even if the only use has been only in breaking down the fear of stigma and accepting help.
It’s helpful knowing others have similar struggles, particularly when some colleagues can be hostile.
I think we often use our work with depressed people to deal with our own feelings of despair. It seems to me that you are someone who has the independence of heart and mind to continue offering effective relationship-based work despite the excessively bureaucratic system. Thanks for sharing your experiences.
A beautifully written, cogent, and heartfelt piece, fully of empathy rather than criticism.
As a frontline children’s social worker and parent suffering from depression but not using public mental health services, I found this interesting, and I identify strongly with your feelings and experiences of your illness.
Let’s all take care of one another.
hi, I’m not sure I wouldn’t share some aspects of my experience with some clients if it were helpful. I’ve shared other personal information at times and it has been seen as increasing understanding and empathy.
We all suffer from mental ill health at some point in our lives. The only difference is some of us are braver than others to disclose it, while the rest of us pretend we are invincible.
As an ex social worker and Children’s Guardian it saddens me to hear that the social work profession still lacks understanding of staff with mental health problems. It really is unacceptable but I remember well the anxiety of colleagues “finding out” about my diagnosis. In the end I left the profession, having no other option due to the lack of support, stigma and really dreadful support from line management and Occupational Health. They basically bullied me out of my post when I needed to take some time off. It is truly unacceptable to be so discriminatory to staff and utterly perverse that it’s social workers doing it with our supposed value base.
And I bet you were an excellent social worker and your loss to the service leaves us all poorer. Thank you for your input, I can’t be the only one who I sorry to hear it and hopes you are someday able to return to it in some way. Best wishes.
Thank you for a fantastic and honest article. I agree that it can feel as though we are not meant to recognise that we too are vulnerable; but of course we are – the nature of the work we do and the relentless nature of the trauma we try to support people through must and should have an impact on us. I think the key is how we rest and recover; we must recognise our own vulnerability but seperate that from the vulnerability we see in the people we work with (service users). I think that if you put my life and family history on paper as a referral to my team (Community Mental Health) my colleagues initial assessment of me might be a negative or concerned one. I have choosen to be open with some colleagues but not others and I am sure this is because I do expect some stigma. I personally feel that my life experiece has been a blessing to my practice but distance from my own difficulties has been equally important. I have never choosen to self disclose about my own or my families mental health difficulties to service users; although I recognise that self disclosure can be a tool. I’m alwaus cautious, whose needs am I meeting if I make a personal disclosure, am I making assumpitons about how that would benefit me if somone told me their story?