
Mental Health Act detention rates are three and a half times higher in the most than the least deprived parts of England, while racial disparities have also widened, new data shows, according to new data
The findings, which show that risk of detention rises steadily with an area’s level of deprivation, has prompted calls from a social work leader to tackle the social causes of mental illness, rather than focusing on individual pathology.
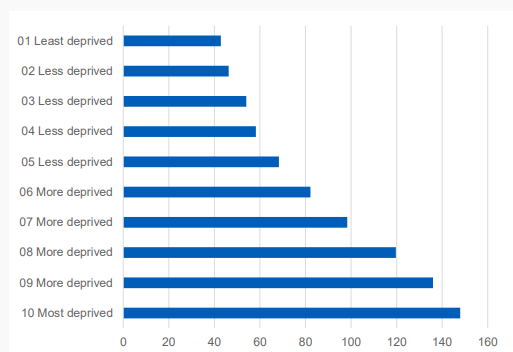
NHS Digital’s 2019-20 Mental Health Act statistics report, the first to analyse detentions based on areas of deprivation, found there were 147.9 detentions per 100,000 people in the most deprived tenth of areas, while the least deprived areas tenth recorded a rate of 42.8 detentions per 100,000. Data for other areas showed a clear link between deprivation and detention risk.
 Issues needs ‘more than just tea and sympathy’
Issues needs ‘more than just tea and sympathy’
Steve Chamberlain, chair of the AMHP leads network, said the findings were unsurprising but should prompt action to tackle the root causes of mental health crisis.
“There is a remarkably consistent relationship between the two and I believe it should prompt more exploration about the impact of socio-economic factors on people’s mental health, as opposed to focusing on individual pathology,” he said.
The issue needs more than “just tea and sympathy”, Chamberlain said, adding: “Given the considerable cost to the economy of mental illness, surely investing in communities is an economically sound strategy, leaving aside the issue of the trauma that individuals experience who are in mental distress.”
Widening racial disparities
The data showed a slight increase in racial disparities in detention rates and a significant rise in inequalities for use of community treatment orders (CTOs).
Known rates of detention for Black or Black British people rose 5% on the previous year, increasing from 306.8 detentions per 100,000 to 321.7 detentions per 100,000. The ratio of detentions for this group compared with white people was 4.38 in 2019-20, compared with 4.21 in 2018-19.
Black or Black British people were over ten times as likely as white people to be subject to a CTO, up from eight times in 2018-19, with their rate rising from 53.8 to 61.3 uses per 100,000, compared with 6.0 per 100,000 for the white group.
Chamberlain said there needed to be a “fundamental change in the proportions” to start addressing racial inequality in mental health.
Providers ‘must keep clear and accurate records’
In total, there were 50,893 new detentions under the Mental Health Act during 2019-20, which was up 1.8% from the 49,988 recorded the previous year.
As with previous years, the accuracy of data was compromised because not all providers submitted data while some submitted incomplete data. Using the subset of providers that submitted good-quality data in each of the last three years, NHS Digital estimated there was a 0.8% increase in detentions from 2018-19 to 2019-20.
Chamberlain said he “continues to be amazed” that NHS Digital is unable to obtain complete data regarding the use of the Mental Health Act.
“Given the enormity of the decisions that are made and the impact on each individual, it seems to me absolutely necessary that each and every provider which has the ability to detain patients or place them under some form of compulsion must keep clear and accurate records and be able to make full returns on an annual basis,” he added.


 Bournemouth, Christchurch and Poole
Bournemouth, Christchurch and Poole  Hampshire County Council
Hampshire County Council  Lincolnshire County Council
Lincolnshire County Council  Norfolk County Council
Norfolk County Council  Northamptonshire Children’s Trust
Northamptonshire Children’s Trust  South Gloucestershire Council
South Gloucestershire Council  Wiltshire Council
Wiltshire Council  Wokingham Borough Council
Wokingham Borough Council  Children and young people with SEND are ‘valued and prioritised’ in Wiltshire, find inspectors
Children and young people with SEND are ‘valued and prioritised’ in Wiltshire, find inspectors  How specialist refugee teams benefit young people and social workers
How specialist refugee teams benefit young people and social workers  Podcast: returning to social work after becoming a first-time parent
Podcast: returning to social work after becoming a first-time parent  Podcast: would you work for an inadequate-rated service?
Podcast: would you work for an inadequate-rated service?  Family help: one local authority’s experience of the model
Family help: one local authority’s experience of the model  Workforce Insights – showcasing a selection of the sector’s top recruiters
Workforce Insights – showcasing a selection of the sector’s top recruiters 

 Facebook
Facebook X
X LinkedIn
LinkedIn Instagram
Instagram
Perhaps if social workers actually worked alongside their ‘clients ‘ to do the boring things to support them in their daily lives rather than stepping in as superheroes when we are in crisis, they too would own the “investing in communities” Mr Chamberlain urges others, yet again, to do. It’s interesting how social workers become impotent and powerless one minute and the fount of knowledge and empowerment when it suits them. How about owning that impotence is a choice? Be honest, you are an integral part of the mental health establishment, you are not a cog. Social workers choose the side of the powerful if meaningful action has negative consequences for them. If the mental health system has racial inequalities then social workers are part of that problem. Stop blaming others for your own complicity as AMPH’s Mr Chamberlain. Start making alliances with the victimised and powerless and stop being the tools of psychiatrists in dehumanising illness and distress. And yes, I am an embittered human being sick of hearing how social workers are justice warriors when in reality most are more interested in the validation of psychiatrists than the likes of me.
Really interesting and powerful comment. Yes, we as social workers and AMHPs cannot wash our hands of responsibility for some of this data, including for example the hugely disproportionate numbers of black people subject to CTO compared to their white counterparts.
And I agree that social workers should also stand up for people who are powerless and should be working alongside their clients.
This data is about much larger economic issues such as unemployment, poverty, inadequate housing.
It indicates to me that people are going to experience mental distress, and some reach mental health crisis, much more frequently if they are living in conditions of socio-economic deprivation and exclusion than if they were in a less disadvantaged environment.
I don’t think that many AMHPs consider themselves ‘superheroes’ or ‘justice warriors’. They undertake an important and incredibly difficult role which includes at times taking away someone’s liberty. This is never an easy decision and it never becomes ‘routine’.
It is particularly difficult to stand by people when they are in mental health crisis and there is a decision to make regarding their possible detention in hospital. I hope that AMHPs always attempt to maximise the person’s ability to have their voice heard and to give them the maximum dignity in circumstances which are almost always ones of high risk and emotion.
Nicjolas as an AMHP I have to say that I agree with you.
Absolutely agree change is needed but this is talked about every year – when are these organisations including NHS going to wake up and do something about it. The same conversation is boring! Reform to MHA is coming so they keep saying but it does little to change culture, lack of data and poor balance of equalities.
That black and white working class people are disproportionately in the formal mental health system elicits a response about paucity of accurate statistics and a polite plea for “more exploration about the impact of socio-economic factors on people’s mental health” says all. We read that a pilot is needed to understand causes and impact of racism from sector leaders and now more prevarication on impact of poverty and powerlessness on mental health. What is it that we don’t know and need to find out still? Apparently we are celebrating 50 years of social services and BASW. I wonder when all the waffle and self congratulations will end and social workers show pride in solidarity rather than in their supposed professionalism. AMHP Leaders Network never improved my experinces as an AMHP so perhaps I am naive to expect them to make a positive impact on the lives of users of services.
I disagree Steve. At every AMHP training I have attended in the 7 years I’ve been an AMHP, I have been overwhelmed by the self importance of some social workers who really do think we do a job no one else can, superhero delusion!, and that we are the only selfless protectors of liberty, justice warrior delusion! Of course working class people will be funneled into a mental health system over rthat is over reliant on Mental Health Act assessments when most crisis interventions are resource led. We need to be honest and actually listen to what service users tell us about their experinces of being detained. I have rarely known AMHP’s challenge resource limitations unless it involves difficulty accessing a hospital bed. When do we talk about let alone practically tackle issues of poverty and the insidioussness of deprivation? Individualising experinces never gets to the root off social and economic deprivation. Why are so many of the people we ostensibly work with in poor housing? What are social workers doing to tackle isolation and victimisation in the communities they work in? Why are we still in thrall to psychiatrists and psychologists most of whom have zero experience of working class lives? As James says, now is the time for alliances and solidarity. We will only empower people once we step out of our internal bubbles. Dipping in and out of peoples lives when they are at their most vulnerable and distressed only goes so far.
I was shocked at the brutal treatment I was exposed to after seeking mental health support. I trained and worked as a CP social worker for ten years and to this day, cannot comprehend how a statutory support system actively seeks to cause further harm.
I expressed my concerns about experiencing racial abuse on a systemic, cultural and personal level and the significant impact it had on my ability to cope due to the deterioration of my resilience. This was in 2016 as the surge in British Nationalism grew and became almost homogeneous.
My concerns, trauma and deteriorating health, completely changed my life but was dismissed and belittled by MH services.
My advocate and I remain shocked to this day, when a Consultant Psychologist called me racist despite no evidence and storming off for me even daring to highlight racial disparities. Several months later, the Black Lives Matter movement echoed my concerns and surprisingly MH services have remained uncomfortably silent.
I have been prescribed literally bin bags full of medications with few reviews or exploration of their ramifications. The self mutilating began after numerous medications were prescribed but has been dismissed and have been left to get on with it.
I was promised CBT, but 4 years later, no one seems ‘qualified’ enough to explore my experiences of racism and its impact.
The professionals involved in my care, raised my risk level to high, despite no evidence of aggression or violence on my part. This led to 20 police officers smashing down my door, spraying me with CS gas and hog tied me off to prison. No further action my risk apparently remains. It’s almost as if they want me to act violently to substantiate their fears.
The Police have sent more officers with shields and batons in an attempt to section me, but fortunately it was a Friday and all the staff assessing me were black or Asian and acknowledged that I was not insane and let me go.
Being black, educated or articulate, does not preclude you from being perceived as a threat to fragile insidious bigots, who revel in limiting life opportunities for certain demographics.
I acknowledge that British Mental Health support is and has always been Eurocentric, however, as a non European with a British passport, I battle every day coming to terms with societal and country abandonment issues. Having to deal with the post Colonial cognitive dissonance of others is exhausting and has greatly reduced my life opportunities and span, drastically.
It’s simple. Are AMHP’s citizens first who happen to be social workers or does being a social worker seperate them from the communities they live and work in? Are we part of or seperate from the lives of people? It’s painful to be confronted with the realities Nicholas articulates but if social work is to have a relevance, we need to listen. It’s how or if we engage in the “much larger issiues” that should define our usefulness, not overblown bureaucratic tasks redefined as “professionalism”. Let SWE, BASW, ADASS and the rest of the bureaucrats have their echo chamber. They are not us.
Social work continues to remain lethargic or reluctant to ameliorate the racial disparities within all sectors it is fundamentally paid to address.
Statutory services remain totally out of touch with service users, staff and the impact of racial abuse. How can those taught the social model of care continue to implement a biased Eurocentric medical model that fails to acknowledge physiological and emotional differences?
Social workers are taught about the disparities within mental health services but continue to work and maintain an overtly racist institution and uphold draconian mental health legislation. Knowing full well, the devastating impact it has on certain demographics. Hypocrisy, oxymoronic or complicit. In the 21st century, It’s just not good enough.
If you train and are educated to uphold high moral standards, whilst blatantly maintaining morally repugnant systems, you are not the solution for positive progression. Social work is stagnant and it’s uncomfortable privilege, guilt and apathy prolongs the implementation of the much needed societal paradigm shift.
Social workers, please get over your inferiority complexes and stop trying to impress psychiatrists with your “medical” knowledge. It’s bad enough being ‘treated’ by psychiatrists who would struggle to give an injection let alone function as a proper doctor. If you feel you need validation from medics give up. We need AMHP’s who have the guts to challenge not psychiatrists not be their doormat.
AMPH’s primarily serve to perpetuate the pretence of “holistic” mental health interventions while psychiatrists and the police get on with controlling the behaviour of people in “deprived areas”. Keith Rotimi is spot on and shames you all
I am an AMHP. I dont have pretensions of excellence, I just try to do my job as competently and sensitively as I can. Some of my collagues believe they should out doctor the psychiatrists and out smart the advocates and lawyers but I don’t believe they do this to show off only to ensure they are listened to and taken seriously. I can not pretend I really understand what it feels like to have your life invaded by a multitude of perhaps unknown people, nor how frightening it must be to be threatend with handcuffing or restraint. To me it’s a pointless squabble to argue who is better at mental health work. I know everybody tries their best. I am saddened by Keith Rotimis appalling experiences and I hope with humility and an open heart we can learn from his comments and improve how we interact with each other.