People are facing longer waits for reablement support as services see referral numbers rise and staffing levels drop, an audit has found.
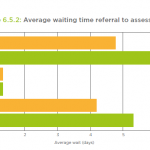
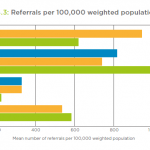
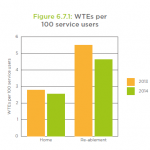
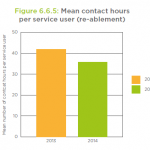
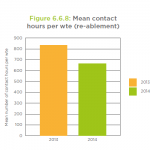
The average wait between referral and assessment was 5.3 days in 2013-14, up from 4.2 days the previous year, found the National Audit of Intermediate Care 2014. The average number of referrals to reablement services rose 9% over the same period but staffing levels dropped from a mean of 5.5 full-time equivalent staff per 100 service users to 4.6, the report found.
Waiting times also worsened in home-based intermediate care services and crisis response services, the audit found. With a high proportion of service users waiting in hospital beds, the waits represented both a ‘lost opportunity’ for efficiency gains in secondary care and a ‘poor care experience’ that damaged patients’ rehabilitation, the report warned.
“A wait of more than two days negates the additional benefit of intermediate care, and seven days is associated with a 10% decline in muscle strength, hardly an advantage for people with frailty for whom muscle weakness is a defining characteristic,” said NHS England’s national clinical director for integration and frail elderly, Professor John Young, in a foreword to the report.
“Perhaps these unnecessary waits in hospital explain the increasing lengths of intermediate care stay reported in the audit, and so the whole system deteriorates.”
Key charts from the report
Shift towards ‘step down’ care
Reablement services provide personal care and daily living support, usually for up to six weeks, in a bid to boost service users’ confidence and skills to live independently. The services offer ‘step up’ support to prevent a person going into hospital and ‘step down’ support for people admitted to hospital to facilitate their discharge and prevent readmission.
The 2014 audit found a marked shift towards ‘step down’ reablement care in 2013-14, with 44% of referrals coming from NHS acute trusts compared to 35% in 2012-13. The trend could reflect the fact that, as part of the government’s Better Care Fund, councils will be monitored on how many older people are still at home three months after discharge to reablement services, the report said.
On average, 82% of service users completed reablement in 2013-14. Following the support, 57% of service users had a reduced ongoing homecare need, 32% had no change and 11% had an increased need, the audit found.
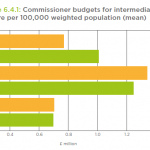
Concerns over capacity
For the third year running, the audit raised concerns over intermediate care capacity. The 2012 audit calculated that capacity needed to double to meet potential demand but the 2014 report found “no evidence” of higher investment in services and said an expansion was “urgently” needed.
The audit found an improvement on some indicators raised as issues of concern in the 2013 report. The proportion of reablement service staff trained in mental health and dementia care rose from 53% in 2013 to 63% in 2014. The number of reablement teams with access to specialist geriatricians rose from 34% in 2013 to 49% in 2014.
About the audit
The audit was produced by organisations including NHS England, the Association of Directors of Adult Social Services and the British Geriatrics Society, which represents specialist older people’s doctors. It received data from 89 CCGs, 47 local authorities and 472 intermediate care services. It also received survey responses from over 12,000 patients and service users.


 Bournemouth, Christchurch and Poole
Bournemouth, Christchurch and Poole  Hampshire County Council
Hampshire County Council  Lincolnshire County Council
Lincolnshire County Council  Norfolk County Council
Norfolk County Council  Northamptonshire Children’s Trust
Northamptonshire Children’s Trust  South Gloucestershire Council
South Gloucestershire Council  Wiltshire Council
Wiltshire Council  Wokingham Borough Council
Wokingham Borough Council  Children and young people with SEND are ‘valued and prioritised’ in Wiltshire, find inspectors
Children and young people with SEND are ‘valued and prioritised’ in Wiltshire, find inspectors  How specialist refugee teams benefit young people and social workers
How specialist refugee teams benefit young people and social workers  Podcast: returning to social work after becoming a first-time parent
Podcast: returning to social work after becoming a first-time parent  Podcast: would you work for an inadequate-rated service?
Podcast: would you work for an inadequate-rated service?  Family help: one local authority’s experience of the model
Family help: one local authority’s experience of the model  Workforce Insights – showcasing a selection of the sector’s top recruiters
Workforce Insights – showcasing a selection of the sector’s top recruiters 

 Facebook
Facebook X
X LinkedIn
LinkedIn Instagram
Instagram
Is there any where I can get a copy of the full audit report?
Hey Russell, it’s Andy from ComCare here (I wrote the story above). I’ve just added in a link to the full report – apologies it wasn’t included in the original story. This is the link: http://www.nhsbenchmarking.nhs.uk/partnership-projects/National-Audit-of-Intermediate-Care/year-three.php
Many Thanks