Social care leaders have voiced concerns over the ending of Covid-19 funding for the sector.
Funding to help care providers fund infection control and Covid testing, and for the NHS to fund free care for up to four weeks for people discharged from hospital with support needs, ended on 31 March, as did winter resources to help providers recruit and retain staff in the face of mounting pressures.
Though the resources were always designed to be time-limited, social care bodies warned their removal carried significant risks for a fragile sector at the height of the latest Covid-19 wave.
‘Adding further pressures to underfunded sector’
A Local Government Association spokesperson said: “The loss of funding streams for social care puts councils and providers onto an even more unstable footing and highlights how volatile the financial situation is within social care. This will only add further pressures to an underfunded sector.
“This pandemic is not over, social care staff continue to do their utmost to keep those who draw on social care safe with limited resources. Ensuring that care providers and councils have the staff and capacity to handle hospital discharges is crucial to ensure people get the right care at the right time, and to freeing up NHS time and space. With less funding this becomes harder and harder to deliver.”
The Homecare Association raised particular concerns about the ending of the infection control and testing fund, which was designed to enable providers to pay care staff off sick or forced to self-isolate and enable care homes to boost staffing levels in order to minimise movement between homes, in order to control transmission of the virus.
“Lack of available infection control funding risks care workers being unable to afford to isolate when Covid-19 positive, particularly as cost of living is escalating,” said chief executive officer Dr Jane Townson.
“We are hearing from providers who currently have up to 30% of their workforce off sick, and therefore unable to provide care for older and disabled people in the community. Workers only become eligible for Statutory Sick Pay after three days, and infection control funding is essential to help providers pay staff as close to a full wage as possible while isolating. Most local authority fee rates for homecare are inadequate to cover normal costs of homecare delivery never mind additional costs due to Covid-19.”
It called on the government to reinstate the funding, which has been worth £1.35bn to adult social care since May 2020, with a further £288m allocated for testing.
Vacancies ‘eye-wateringly high’
From a staff perspective, UNISON voiced similar warnings.
“Scrapping the financial support for sick pay in care, just as the devasting cost-of-living crisis intensifies and Covid rates rise, is negligent and morally wrong,” said head of social care Gavin Edwards.
“With care job vacancies already eye-wateringly high, the government should be encouraging and rewarding staff for doing the right thing by isolating, not making it impossible for them to put food on the table. Workers are already turning to food banks as budgets are stretched to breaking point.
“Ministers must immediately reinstate the infection control fund and make it mandatory for care employers to pay proper sick pay. Anything less will drive more staff out of the sector and put lives and livelihoods at risk.”
Related articles
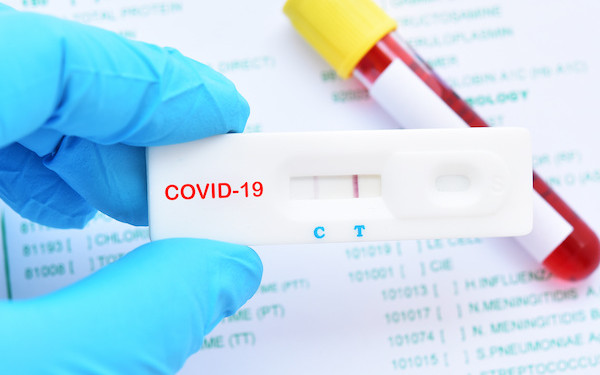
The government has published updated guidance on infection control and prevention in adult social care, a supplement to which states staff should stay off work if they test positive for Covid-19 or have any of the core systems (a new continuous cough, a high temperature or a loss or change in their sense of taste or smell). They should only return following two negative lateral flow tests on consecutive days, at least five days after they tested positive or developed symptoms.
Care homes should not normally have to limit movement between homes but may be asked to by the local director of public health or health protection team if there is high prevalence of Covid-19 locally or an outbreak in a home.
End to discharge funding
Though the national discharge fund – worth almost £3bn over the past two years – has been channeled through the NHS, it was designed to fund free care for people who left hospital with needs. This was designed to speed up discharges using the discharge-to-assess approach, under which people’s ongoing care and support needs are assessed after leaving hospital, ideally in their own home.
In a letter to health and social care leaders last month, NHS England and NHS Improvement (NHSE/I) encouraged them to continue the arrangements for free care using other funding streams, such as the Better Care Fund. The BCF is designed to promote health and social care integration, fund out-of-hospital care and improve hospital discharge, with the NHS being required to put £4.26bn into local pooled funds in 2021-22.
However, in the letter, NHSE/I director of community health Matthew Winn admitted post-discharge capacity may reduce in some areas.
“It is understood that in some areas capacity for post-discharge services may decrease; however, local discharge arrangements have matured in many areas, and we would encourage local systems to continue to embed discharge to assess approaches where affordable within core local funding, with the national Hospital Discharge Programme continuing to provide guidance and implementation support to systems.”
The Department of Health and Social Care has produced revised guidance on hospital discharge, which said it was up to local health and social care leaders to “agree the discharge models that best meet local needs that are affordable within existing budgets”.
It added: “Where local areas agree to fund a period of care (pending a long-term needs assessment being carried out), agreements should be in place to ensure no one is left without care or – if needed – an assessment of long-term needs prior to the end of this period. This should also ensure that no carers are left without adequate support or an assessment of their longer-term needs (if needed) at the end of this period.”


 Family help: one local authority’s experience of the model
Family help: one local authority’s experience of the model  ‘I spent the first three months listening’: how supportive leadership can transform children’s services
‘I spent the first three months listening’: how supportive leadership can transform children’s services  How senior leaders in one authority maintain a culture of excellence
How senior leaders in one authority maintain a culture of excellence  How staff support ensures fantastic outcomes for children and families
How staff support ensures fantastic outcomes for children and families  Workforce Insights – showcasing a selection of the sector’s top recruiters
Workforce Insights – showcasing a selection of the sector’s top recruiters 

 Facebook
Facebook X
X LinkedIn
LinkedIn Instagram
Instagram
[…] April: Government Covid funding for adult social care ends (Community […]