The Association of Directors of Adult Social Services (ADASS) has called for an emergency initiative to bolster the social care workforce after its president warned that the sector risked being overwhelmed by the immense pressures on the NHS and staffing shortages.
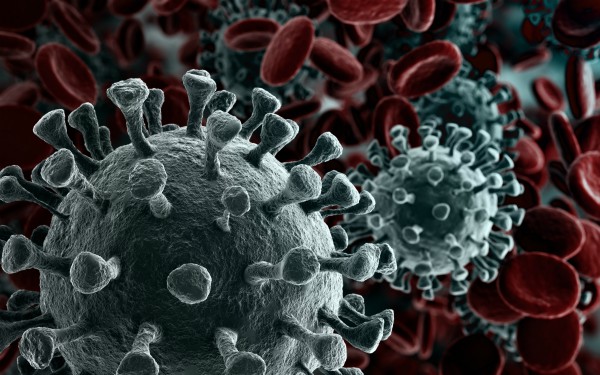
With the number of hospital patients with Covid-19 well exceeding April’s first peak, NHS leaders have called for capacity to be found in the social care sector to relieve pressures on the health service. However, social care providers have warned that capacity has been sapped by high levels of staffing absence and additional pressures created by increased coronavirus testing.
In a tweet yesterday, ADASS president James Bullion warned that the “immense pressures” on the NHS could easily overwhelm social care”, having flagged last week the severe impact staff sickness was having on the sector.
Emergency plan needed
ADASS has now called for “an emergency winter workforce initiative” to attract people into the sector, offering pay and reward incentives and guaranteed immediate vaccination, the precursor to a “national care wage” of at least £10.90 an hour, well above the current minimum of £8.72.
ADASS vice-president Stephen Chandler said: “With steeply rising unemployment, this is a once-in-a-lifetime opportunity to attract a new generation into careers in the care sector and ease its chronic recruitment problems at a stroke.”
Against the backdrop of sector vacancies of 112,000 as of last year, provider bodies told Community Care that the latest phase of the pandemic was making matters much worse.
Absence rates up to 35% in some services
The National Care Forum (NCF), which represents not-for-profit providers, said some members were reporting absence rates of between 25% and 35% in their services.
A spokesperson said this was being driven partly by the increased use of rapid lateral flow device testing but also by increased transmission.
Related articles
Councils face £500m adult social care overspend in 2020-21 as Covid fuels mounting need
Extra £1.7bn for social care needed this winter to tackle shift away from care homes, warns ADASS
Covid-19 drive to clear hospital beds left some of those discharged with unmet needs and no support
Colin Angel, policy director at United Kingdom Homecare Association, said the introduction of weekly testing of home care staff was having similar results.
“[Staff absence has] no doubt increased as asymptomatic workers can now be identified through weekly testing, which has not been available to the home care workforce until recently,” he said.
He added: “The re-introduction of shielding will inevitably have an impact on the capacity of the home care workforce, as a proportion of care workers are now likely to be required to shield again.”
Vaccination impact
Looking ahead to the rollout of vaccinations among home care staff, Angel said this risked exacerbating workforce pressures if not accompanied by additional support.
“Care workers are likely to be required to travel some distance for the vaccination, taking time out of the working day,” he said.
Angel also urged careful planning for how people who use home-based care will receive their vaccinations.
“Many people using home care will require their vaccine to be administered at home, they will either require a care worker to be present to enable access and egress to the home, or (in the absence of informal carers to do so) to accompany people to a vaccination centre,” he said.
“Councils and the NHS will need to think about how such a service could be commissioned quickly.
“There cannot be an assumption that care workers will just be able to sit and wait for the vaccination team to turn up.”
Concerns over family carers
There are concerns too for the resilience of family carers, many of whom are exhausted after months of carrying out caring responsibilities with little respite.
In response, ADASS is calling for an extra payment of £50 a week for carers in receipt of carer’s allowance, while the Covid-19 crisis continues, in order to fund respite breaks.
“If we do nothing and leave thousands of family carers to burn out, the costs to the state will be incalculably higher than those of providing a modest sum in extra support,” Chandler added.
Significant lack of Covid-secure homes
Meanwhile, 51 of 151 local authorities are yet to identify at least one Covid-secure home, under the designated setting scheme.
Councils, providers and the NHS are working to identify at least one care home in every local authority area to which people who have tested positive for coronavirus can be discharged to from hospital and cared for, for the remainder of the required isolation period.
The Care Quality Commission (CQC) must first inspect the “designated setting” and ensure it meets the latest infection prevention control standards.
CQC data shows that, as of 29 December, only 42% of London councils had at least one approved setting, with a similarly grim picture in the South West, where less than half of councils are yet to identify a Covid-secure home.
“We’re in discussion with the Department of Health and Social Care (DHSC), and system partners to address issues of capacity across the country, particularly in areas where there is a shortage or lack of designated settings,” the regulator said.
‘Immensely proud’ of care staff
In response to the concerns, a DHSC spokesperson said: “We are immensely proud of all our care workers do and recognise their tireless work on the frontline of this pandemic.
“Since the introduction of the National Living Wage, care worker pay has risen at a faster rate than ever and throughout this pandemic we have made sure care workers are properly supported financially, including ring-fencing over £1.1bn of funding which can be used to pay staff who may need to self-isolate.
“We know there is a need for a long-term solution for social care and are looking at a range of proposals as part of our commitment to bringing forward a plan that puts the sector on a more sustainable footing for the future.”


 Bournemouth, Christchurch and Poole
Bournemouth, Christchurch and Poole  Hampshire County Council
Hampshire County Council  Lincolnshire County Council
Lincolnshire County Council  Norfolk County Council
Norfolk County Council  Northamptonshire Children’s Trust
Northamptonshire Children’s Trust  South Gloucestershire Council
South Gloucestershire Council  Wiltshire Council
Wiltshire Council  Wokingham Borough Council
Wokingham Borough Council  Children and young people with SEND are ‘valued and prioritised’ in Wiltshire, find inspectors
Children and young people with SEND are ‘valued and prioritised’ in Wiltshire, find inspectors  How specialist refugee teams benefit young people and social workers
How specialist refugee teams benefit young people and social workers  Podcast: returning to social work after becoming a first-time parent
Podcast: returning to social work after becoming a first-time parent  Podcast: would you work for an inadequate-rated service?
Podcast: would you work for an inadequate-rated service?  Family help: one local authority’s experience of the model
Family help: one local authority’s experience of the model  Workforce Insights – showcasing a selection of the sector’s top recruiters
Workforce Insights – showcasing a selection of the sector’s top recruiters 

 Facebook
Facebook X
X LinkedIn
LinkedIn Instagram
Instagram
Lets not forget about all the social workers in and out of people’s homes, in and out of care homes. Whilst NHS workers are getting vaccinated, everyone seems to have forgotten about social workers!!
Not forgotten at all here, but it seems to be very specific to localities. Some SWs in another borough were offered the vaccin 2 weeks ago and our service was last week. We do some frontline work when essential, but mostly spend our days pyjama working from home. We were offered vaccin slots before a team that does community rehab we later found. So go figure local decisions!
Its shameful of Stephen Chandler to use unemployment as an “opportunity” to further exploit workers. I have news for him, desperation and poverty is not a moral nor a sustainable recruitment model. That ADASS thinks £10.90 an hour is a fair wage for care workers says all. This year council tax is set to rise by 20% in most metropolitan authorities, food prices are likely to rise post Brexit, fares are set to rise more than inflation in London. Perhaps we can be told how many ADASS staff are paid £10.90 an hour. I recall ADASS advocating for massive injection of tax payer funds into the pockets of hedge funds last year. Can we please have the same enthusiasm on behalf of workers rather than advocating for continued low pay. I seemed to have missed any comment by ADASS on the £43 million paid out in dividends to the share holders of HC-One. How about ADASS having a word so that a fraction of obscene dividend pay outs can be reserved for sustained decent pay and conditions. Perhaps that is the once in a life time opportunity for a recruitment strategy that will ensure stability in the sector.
When our own managers and our own regulator ignore us, why do you expect others to remember you Doncaster? Actually it’s not a race about who is the most deserving. Unlike social workers, most care workers have multiple jobs and are in and out of many more doors than us. My partner being one. I wonder why she has suddenly come to the attention of ADASS? The cynic in me questions their sudden concern for care workers. Can we be told how much of, if any, of the additional funding for staff absence and infection control has been used for that purpose by your chums ADASS?
When even the Daily Mail railes against the pay rise of a provider boss, can we really believe that ADASS is fit for purpose?
Looking forward to ADASS letting us know how the second additional funding £120m has been spent.
Any explanation ADASS for the 64% increase in care home deaths since the first tranche of money was dished out for PPE, infection control and staff costs?